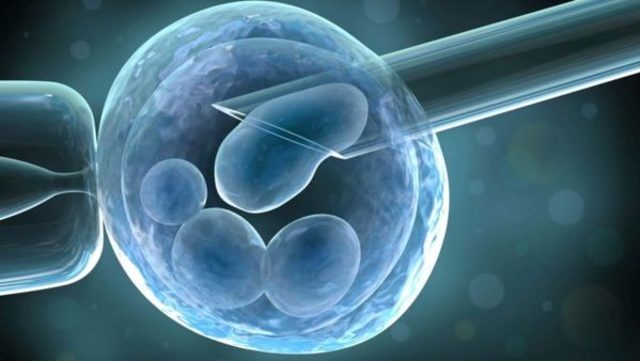
Intrauterine insemination (IUI) is a procedure designed to place sperm directly into a woman’s uterus through artificial means. The sperm is prepared for this procedure in the laboratory and then deposited inside the endometrial cavity using a small catheter passed through the endocervical canal.
IUI is recommended for patients:
- who has anovulatory disease such as polycystic ovarian syndrome (PCOS)
- in whom the partner’s sperm production has decreased or the motility of the sperm has been compromised
- who have unexplained infertility (normal infertile couples)
- who have a history of mild to moderate endometriosis after laparoscopic treatment
IUI can be performed during a natural ovulation cycle, or with ovulation induction with some pills taken orally and some injections. In general, after the administration of the ovulation induction medication, the follicular development is monitored by pelvic ultrasound and sometimes by estradiol and LH determination in blood.
Once the time of ovulation is predicted, a semen sample will be produced by the partner in the andrology lab. The semen is processed through the special technique known as sperm wash, which consists of incubation and separation of the sperm to obtain the best quality sperm. The final sample will be placed inside the endometrial cavity using a catheter specially designed for IUI.
IUI: Intrauterine Insemination
The IUI Treatment Program at San Diego Fertility Center
Intrauterine insemination (IUI), also known as artificial insemination, is a fertility procedure in which sperm are washed, concentrated, and injected directly into a woman’s uterus. The most common indications for IUI are cervical mucus abnormalities, low sperm count, low sperm motility, increased sperm viscosity or antisperm antibodies, unexplained infertility, and the need to use frozen donor sperm. In natural intercourse, only a fraction of the sperm make it past the woman’s cervical mucus into the uterus. IUI increases the number of sperm in the fallopian tubes, where fertilization takes place.
Studies show that IUI, or artificial insemination, is most successful when it is coupled with fertility drugs that recruit multiple follicles. This technique often is called controlled ovarian stimulation and IUI.
IUI sometimes is recommended for couples with unspecified infertility who have been trying to have a baby for six to 12 months. You should have a thorough infertility evaluation before trying IUI.
Male Partner Requirements for IUI
IUI relies on the natural ability of sperm to fertilize an egg in the fallopian tubes. Studies show that IUI will not be effective in cases where the male has low sperm counts or poor sperm shape (also known as sperm morphology). Sperm tests are required, therefore, in order to indicate:
- Sperm count (number of sperm per cc)
- Sperm motility (percentage of sperm moving)
- Sperm morphology (shape)
the male (or female) partner must also have blood work done to rule out certain infectious diseases.
Female Patient Requirements for IUI
The patient should have normal hormone test results, open fallopian tubes, and a normal uterine cavity.
- Women with ovulatory disorders can be candidates for IUI if they respond adequately to fertility drugs. In these cases, hormone treatments stimulate follicle growth and the IUI is timed to take place after ovulation is induced. Hormone treatments are usually used even for women without an ovulatory disorder.
- Women with mild endometriosis may benefit from IUI if they do not have a distortion of the pelvic structures.
- Women with severely damaged or blocked fallopian tubes are not candidates for IUI.
Intrauterine Insemination Procedures
IUI is timed as closely to ovulation as possible, therefore we will control the time of ovulation with the administration of hCG (ovulation trigger injection). The insemination is accomplished by placing a speculum in the vagina to visualize the cervix. A small, sterile catheter containing the sperm will be inserted through the cervical opening into the uterine cavity next to the tubal openings. You may experience some spotting or light bleeding after the insemination, which is normal; however, we do ask that you avoid any strenuous exercise on the day of your insemination.
Clomiphene citrate and FSH IUI
Clomiphene citrate IUI and follicle stimulating hormone (FSH) IUI are techniques that require the use of fertility drugs. Clomiphene citrate, human menopausal gonadotropins (Menopur), or purified human FSH (Gonal-F, Follistim, or Bravelle) have been used to induce a condition of superovulation. When these drugs are prescribed, the expected result is an increase in the number of ovulated eggs per cycle, thus increasing the likelihood of fertilization. Fertility drugs also may increase the efficiency of folliculogenesis and may improve subtle luteal phase insufficiencies.
Benefits and Success Rates of IUI
The success rates of superovulation (from hormone treatment) with IUI are between 5 and 20 percent per cycle (depending on the woman’s age and egg quality) provided that the male partner’s sperm count is within normal limits and the female’s tubes are healthy.
The use of hMG or FSH either alone or in combination with intrauterine insemination has been shown to significantly increase cycle fecundity. Overall, the best results are seen when these drugs are used together with IUI.
Doctors might try up to three cycles of IUI, and if these are not successful, recommend more advanced fertility treatment methods such as In-Vitro Fertilization (IVF). Unlike IVF, IUI does not involve egg collection or IV sedation.
